A dental implant is a medical device that is implanted into the jawbone to replace the root portion of a missing tooth. These orthopedic root form devices were originally developed in Sweden and Switzerland in the 1970s and are comprised of titanium metal which mechanically bonds to human bone. Dental implants have been used to replace teeth for over 50 years, and during that period have enjoyed the highest success rate ever recorded for any medical device inserted into human bone. Today, dental implants are the standard of care for tooth replacement providing clinical benefits that exceed a natural tooth (see Table 1).
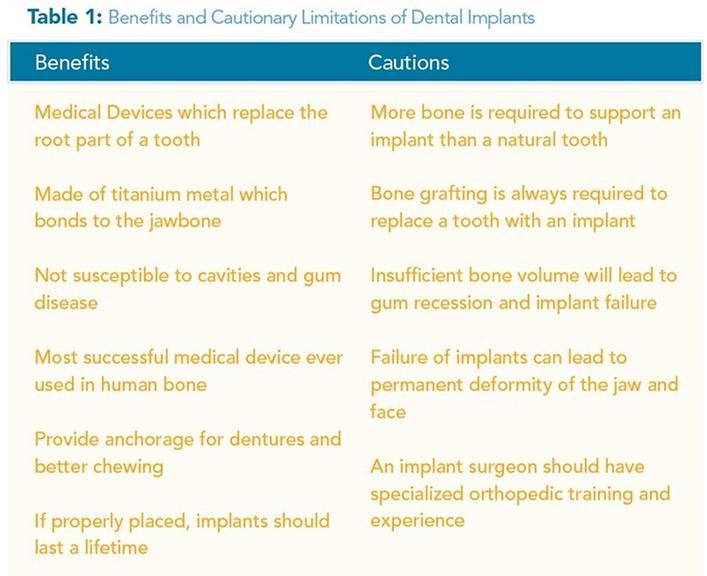
Dental implants were introduced in the United States in 1985 with very meticulous placement protocols and sterile field requirements. The placement of dental implants was only permitted by dental surgical specialists who had been rigorously trained in the necessary orthopedic procedures. For the first 30 years of implant dentistry in this country, dental implants placed by orthopedic surgical specialists enjoyed a reputation of excellence, predictability, and sustainability. Recently, this trend of success has been endangered by dental implant placement performed by inexperienced general dentist practitioners who have not received formal orthopedic surgical training.
Dental implant failure and jaw deformities are two common complications of improper implantation. Three to six years of specialized orthopedic training in an ADA-recognized Specialty Program (Periodontics, Oral Surgery) is required to perform oral surgery, bone graft, and dental implant placement into bone. It is imperative to realize before selecting a dental implant specialist that the dental profession allows general dentists to perform a broad range of surgical procedures without formal surgical training. Weekend classes or minicourses are not the kind of certification you should feel comfortable with from any practitioner within your healthcare team. Be assured of your practitioner’s level of specialty training, years of experience, and track record of success by checking their credentials. This is the first benchmark in assuring that your dental surgical specialist is knowledgeable and capable of offering you a high standard of care.
Dental implants have been used to replace teeth for over 50 years, and during that period have enjoyed the highest success rate ever recorded for any medical device inserted into human bone.
The purpose of this article is to inform the community of the Central Valley about what is necessary for proper surgical placement of an orthopedic dental implant into the bones of the skull. An informed public will be better able to make dependable health decisions and thereby avoid injury and jaw deformity.

Understanding Tooth Removal and Bone Repair
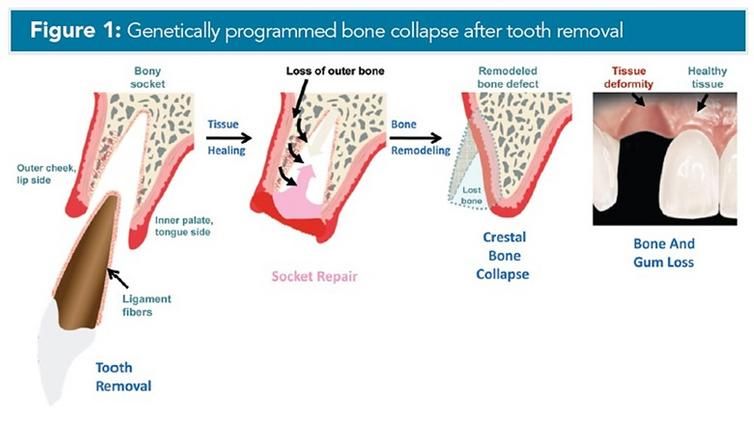
Dental implants were designed to fit into the bone region that formerly housed the tooth that was lost, damaged or removed. An understanding of tooth anatomy and the biologic process of bone repair is vital to grasp the scientific principles of dental implant therapy. A natural tooth is anchored to the jawbone via ligament fibers that connect the root portion of the tooth with the wall of the bony socket. Removal of a tooth from the jawbone always results in remodeling of the bony socket leading to bone collapse at the removal site. It has been observed that most of the crestal bone loss occurs on the outside of the jawbone that faces the cheeks or lips. A lesser amount of bone loss occurs on the palate or tongue side of the jawbone (see Figure 1).
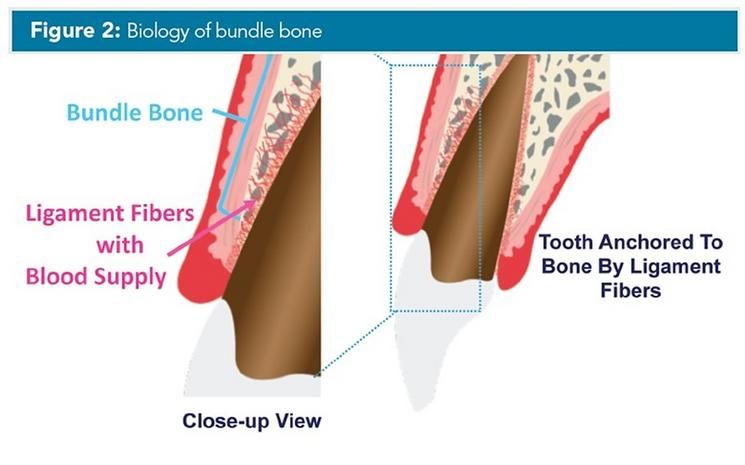
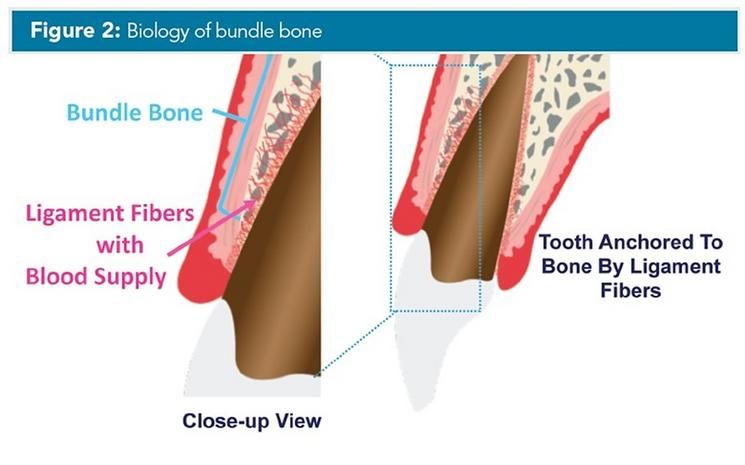
Recent bone healing research has determined that after tooth removal, a bony ridge deformity occurs from the remodeling process resulting in crestal bone collapse. The outer edge of the bone wall is occupied by a genetically-derived bone type called “bundle bone.” The tooth is anchored to the bundle bone and is invested with ligament fibers that provide a vital blood supply to this delicate bone wall (see Figure 2).
Tooth removal results in the loss of tooth ligaments that provide essential bone nourishment. With the removal of the tooth and ligaments, the blood supply to the bundle bone is severed and the bone begins to dissolve away. The bone crest rapidly collapses and is reabsorbed leaving a bony deformity. Because bundle bone is found primarily in the thinner more delicate outer bony region, bone tissue loss will become most pronounced in the highly visible cheek and lip side of the tooth socket. Bundle bone is a tooth-dependent tissue and will always rapidly disappear after tooth removal.
Always Increase the Bone Volume
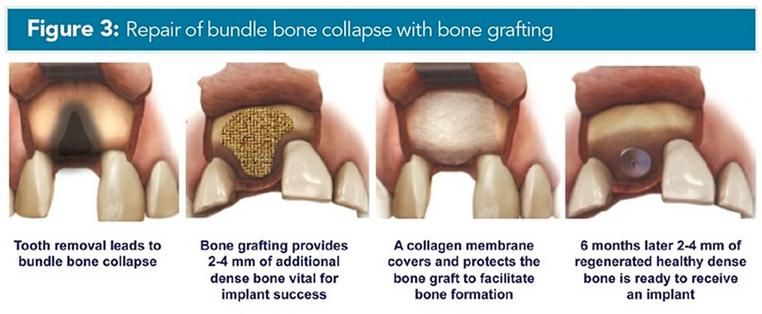
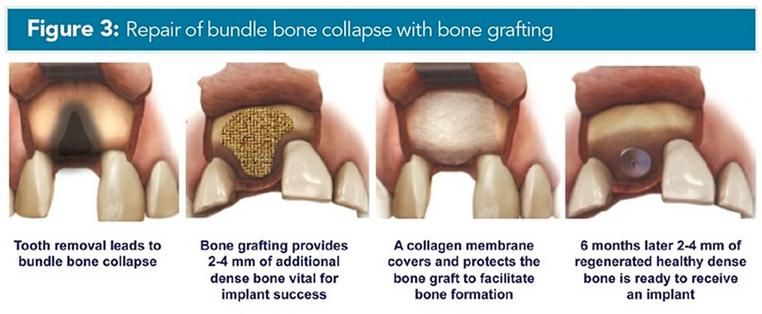
The only way to prevent bone loss at the time of tooth removal is to graft the bony socket with natural bone in combination with a grafting material that will help to preserve and thicken the local bone volume. If bone grafting is not performed, there will not be a sufficient bone volume available to successfully support a dental implant or provide a great result. Clinical research has demonstrated that a significantly greater amount of bone volume (2-4 mm) is required to maintain a dental implant than is required to house a natural tooth. This large amount of bone thickness required for anchorage of a dental implant does not normally exist and has to be created. Consequently, bone supplementation is a necessity if an implant is to be considered. Since the bundle bone is rapidly lost due to a programmed ridge collapse, bone grafting should ideally be performed at the time of tooth removal. A tooth removed without the benefit of immediate bone grafting may still be repaired at a later time but will likely be more extensive and costly. After bone grafting has been performed, a period of at least 6 months is required for the bone to grow and harden prior to placing a dental implant (see Figure 3).
Surgical specialists with advanced orthopedic training in dental implants are proficient at growing bone and utilize the most advanced materials and latest techniques to create bone volume for dental implant support. Expertise in all the following steps is required for successful bone growth:
- harvesting of natural bone chips
- use of platelet-derived growth factors
- selection of appropriate graft material and collagen membrane
- graft preparation and membrane placement
- specialized orthopedic surgical experience
- a thorough scientific knowledge of bone biology.
Questions that you should ask when selecting your dental implant specialist include:
- What type of orthopedic specialty training in dental implants and bone grafting have you received?
- How long have you been placing dental implants?
- How many dental implants have you placed over your career?
- Do you place dental implants immediately into extraction sites?
- What is the scope of bone graft training you have received?
- Do you believe bone grafting is necessary?
- How will you know if I have enough bone for a dental implant?
- Do you require a CBCT-scan to do your dental implant diagnostic planning?
- Do you use CBCT-rendered surgical guides for dental implant positioning?
- How do you develop the gum tissue around the dental implant?
- How well do you work with my restorative dentist?
Avoid Immediate Implant Placement
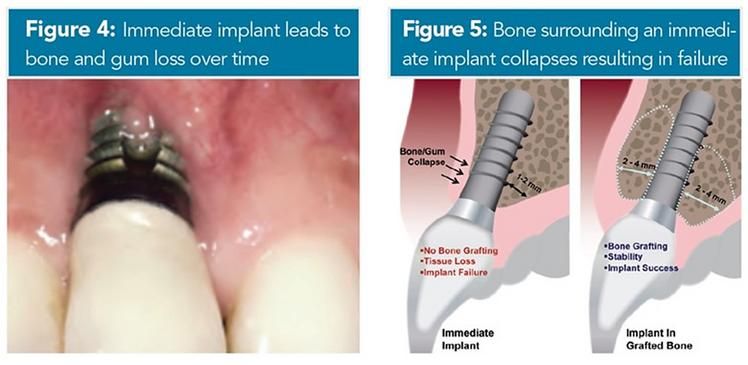
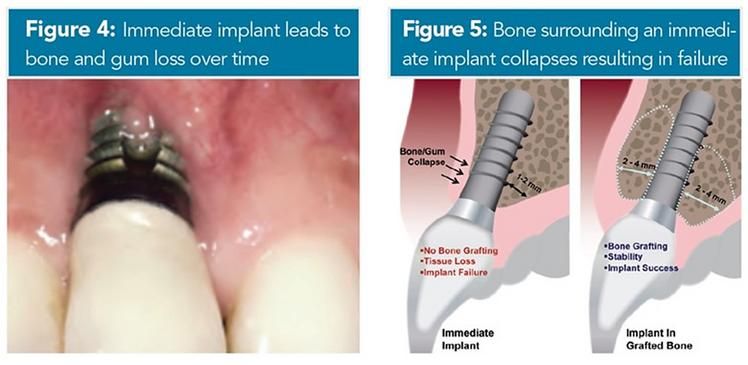
In an effort to circumvent bone grafting, many general dentists have attempted to insert a dental implant into the bone socket at the time of tooth removal. This process is called immediate implant placement, “same day implants” or “implants in a day.” Initially, it was believed that dental implant placement at the time of tooth removal would prevent bone socket collapse. However, recent clinical research has conclusively proven that placing a dental implant into a fresh socket cannot prevent collapse of the bony ridge. The bone does not “see” the dental implant and therefore bone remodeling is not influenced by the dental implant device. Bundle bone was lost following dental implant installation due to the genetically programmed collapse. A dental implant is unable to substitute for a tooth immediately following removal and cannot meet the biologic demands or provide the essential blood supply required to retain the delicate bundle bone. It is now well established that dental implant placement immediately into fresh tooth sockets results in loss of the outer bone covering the dental implant and the metal on the dental implant surface becomes exposed. This bundle bone collapse results in gum recession, esthetic concerns and ultimately dental implant failure (see Figure 4).
Immediate dental implant placement has been primarily abandoned by the leading specialists in the field of implant dentistry. Some sites can receive an immediate implant if the wound bed is buried at time of dental implant placement. Immediate dental implant treatment requires exceptional skills, advanced knowledge of bone biology and careful case selection. These skillsets and knowledge are learned in ADA-recognized surgical specialty dental implant training residency.
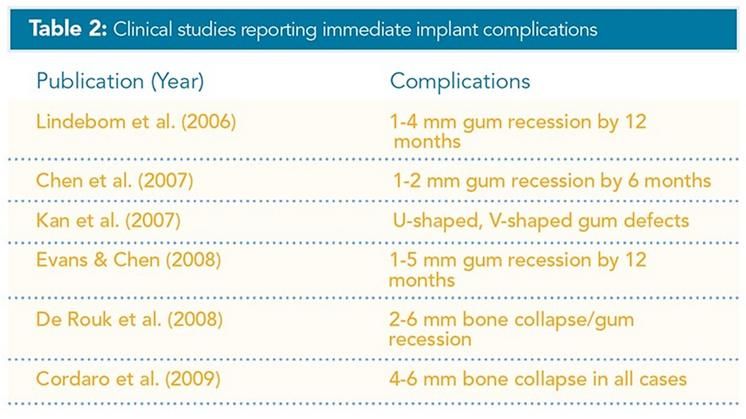
Several studies have reported unsightly results due to bundle bone collapse and gum recession as soon as 6 months after dental implant placement (see Table 2). This immediate approach to dental implant placement is no longer considered a first line standard of care because of the high incidence of unsatisfactory results and complications that lead to jaw deformity including additional tooth loss. If a tooth is to be extracted, it is critical that bone grafting be performed to prepare the site by increasing the bone volume prior to replacement with a dental implant (see Figure 5).
Efforts to skip the bone building process by immediate insertion of the dental implant will always lead to bone collapse, esthetic nightmares, chronic tissue infection, and eventually implant failure. For successful implantation, it is important to take the time required to complete the necessary steps to achieve a dental implant result that lasts.
Standard of Care for Dental Implant Planning and Placement
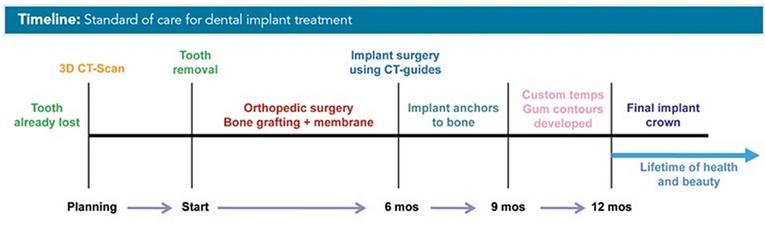
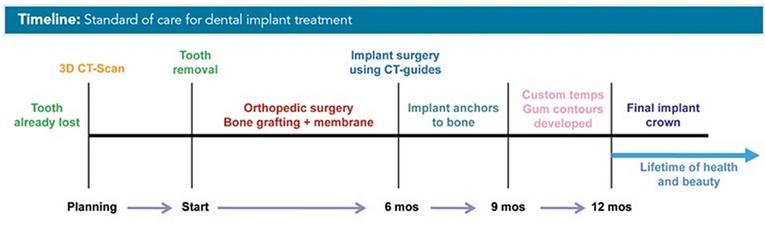
It is clear that bone sets the stage for successful dental implants. Therefore, it is essential that bone architecture, volume and density, in addition to the location of nerves and sinus cavities, be assessed prior to dental implant surgery. Since the jawbone is covered by gum tissue, it is impossible to accurately examine the bone structure without the application of CT-scan technology. In the last two decades, breakthrough scientific advances in x-ray imaging have led to the development of Cone Beam CT equipment (CBCT) and software that precisely reveal this vital information in three-dimensions (3D) using a very low radiation dosage. The accuracy of this technology is astounding and affords the clinician the opportunity to do extensive diagnosis, planning and preparation prior to tooth removal, bone grafting and dental implant surgery.
Today, proper diagnosis and planning includes 3D-CBCT-imaging of all proposed implant sites.
3D CBCT-imaging is an essential standard of care for anyone considering dental implant therapy and allows the dental implant team to define parameters of care, treatment limitations and costs pre-operatively. Just as an orthopedic surgeon would not perform a hip or knee replacement without extensive CT imaging and calculations, dental professionals should not proceed with placement of an orthopedic dental implant without CBCT-imaging and precise positional calculations. Traditionally, dentists have mistakenly used standard dental x-rays and mouth molds to determine bone volume and dental implant position. Today, proper diagnosis and planning includes 3D CBCT-imaging of all proposed dental implant sites (see Figure 6).
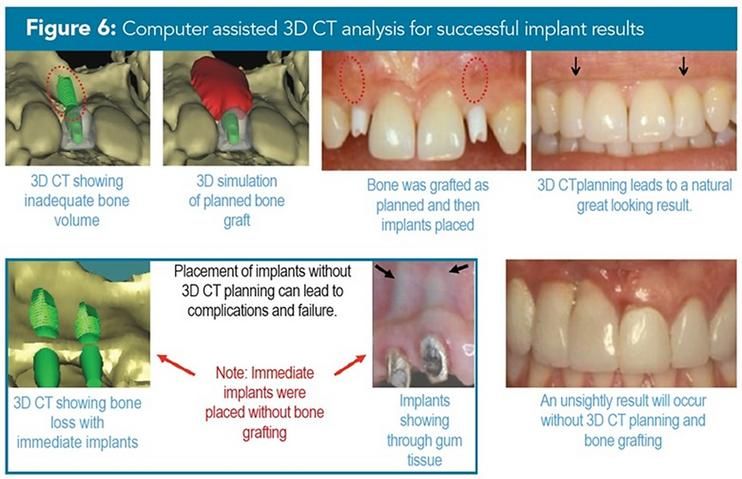

This approach permits 3D site planning for engineering bone and gum tissues and determines all possibilities for proper dental implant positioning and alignment. 3D CBCT analysis and planning changes the surgical approach from speculation to an accurate simulation of the surgery to come. This precise survey permits the surgeon to plan and virtually perform the dental implant surgery in advance, defining in 3D the esthetic and functional demands and costs for dental implants. Once a thorough 3D CBCT examination has been performed, needed bone may be engineered to support a dental implant. Creation of new bone requires approximately 6 months for maturation at which time placement of a dental implant may be considered. Using 3D CBCT data revealing the newly grown bone, precise implant angulation can be determined.
Once the surgeon has defined the ideal dental implant position, customized positioning guides may be constructed from the configured CBCT-data for use during dental implant surgery. The 3D CBCT rendered surgical guide fits upon the adjacent teeth for stability, and precisely guides the dental implant surgeon to deliver the dental implant with proper depth, alignment angle, and positional relationship to the nearby teeth. 3D CBCT-rendered surgical guides permit accurate delivery of this orthopedic medical device into the ideal position for function and beauty. Using surgical guides eliminates misalignment errors and mal-positioning of dental implants thereby reducing complications, undesirable results and dental implant failure. Dental implant placement too close to a nearby tooth will result in loss of bone on that tooth and lead to an unsightly result and eventual tooth loss. For a dental implant to be successful, the standard of care requires precise dental implant placement using such computer-guided technology.
Framing The Tooth
Once a dental implant is properly placed, a period of 2-3 months is required for union of this orthopedic device with the bone. The next step is to develop the gum tissue around the implant so that it will adapt to the final porcelain crown which simulates a natural tooth (see Figure 7).
No one individual can master all the steps and all the complexities of the implant process. Find out for yourself who is most qualified to provide the excellence you deserve when considering implants.
The purpose of gum tissue is to cover and protect the jaw bone from the mouth and to form a seal around teeth. If a smaller volume of bone is present, then there will also be a smaller amount of gum tissue framing a tooth. Similarly, gum tissues also form a seal around dental implants protecting the bone which is in union with the implant. Because gum tissues around a dental implant have a reduced blood supply and supporting fiber network when compared to a native tooth, it is very difficult to make a dental implant tooth look like a real tooth. In order to create sufficient amount of gum tissue to frame a dental implant, it is necessary to engineer an appropriate bony tissue base as described earlier. Newly created bone with orthopedic grafting provides a nourishing framework that supports the gum tissues that encase a dental implant crown. The gum tissue bed that frames the crown is shaped and contoured using customized acrylic temporaries over a period of several months. Exquisite temporary crowns must be modified every few weeks to develop a natural gum geometry surrounding the dental implant.
Choose A Dental Implant Surgical Specialist
Finding the right team is essential to a successful dental implant experience (see Table 3).
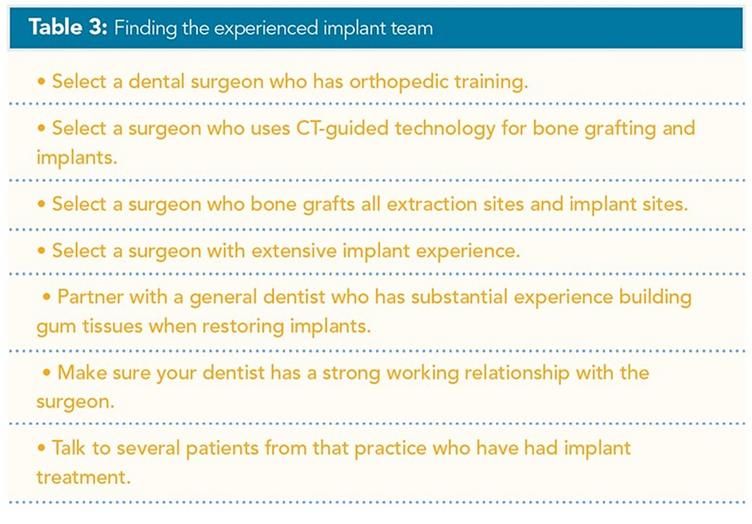
Since bundle bone always collapses after tooth removal and bone grafting is essential for dental implant support, it is critical that you find an experienced team that includes a dental implant surgical specialist with orthopedic training (Periodontics and Oral Surgery). Another vital member of the team is a knowledgeable general restorative dentist with proven experience in building gum contours when restoring dental implant crowns. No one individual can master all the steps and all the complexities of the dental implant process. Find out for yourself who is most qualified to provide the excellence you deserve when considering dental implants. Do your own research, seek multiple opinions and ask the specific questions that help you discern the best dental implant specialist for your dental implant needs.
A dental implant is a medical device that is implanted into the jawbone to replace the root portion of a missing tooth. These orthopedic root form devices were originally developed in Sweden and Switzerland in the 1970s and are comprised of titanium metal which mechanically bonds to human bone. Dental implants have been used to replace teeth for over 50 years, and during that period have enjoyed the highest success rate ever recorded for any medical device inserted into human bone. Today, dental implants are the standard of care for tooth replacement providing clinical benefits that exceed a natural tooth (see Table 1).
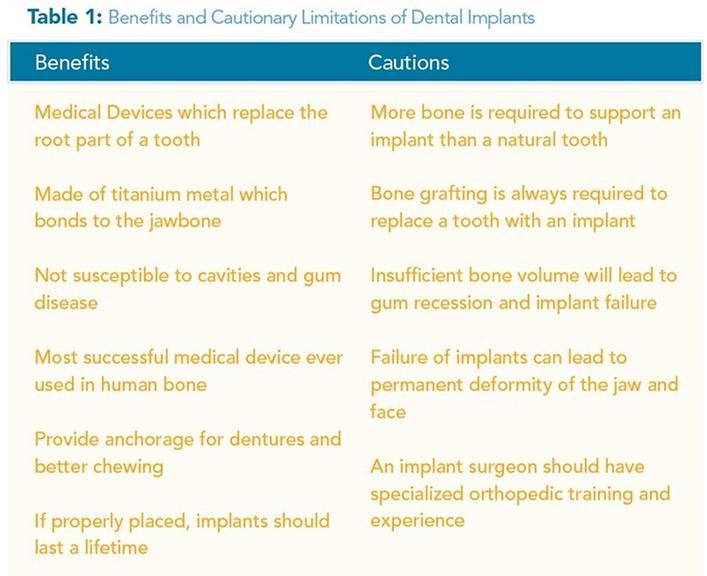
Dental implants were introduced in the United States in 1985 with very meticulous placement protocols and sterile field requirements. The placement of dental implants was only permitted by dental surgical specialists who had been rigorously trained in the necessary orthopedic procedures. For the first 30 years of implant dentistry in this country, dental implants placed by orthopedic surgical specialists enjoyed a reputation of excellence, predictability, and sustainability. Recently, this trend of success has been endangered by dental implant placement performed by inexperienced general dentist practitioners who have not received formal orthopedic surgical training.
Dental implant failure and jaw deformities are two common complications of improper implantation. Three to six years of specialized orthopedic training in an ADA-recognized Specialty Program (Periodontics, Oral Surgery) is required to perform oral surgery, bone graft, and dental implant placement into bone. It is imperative to realize before selecting a dental implant specialist that the dental profession allows general dentists to perform a broad range of surgical procedures without formal surgical training. Weekend classes or minicourses are not the kind of certification you should feel comfortable with from any practitioner within your healthcare team. Be assured of your practitioner’s level of specialty training, years of experience, and track record of success by checking their credentials. This is the first benchmark in assuring that your dental surgical specialist is knowledgeable and capable of offering you a high standard of care.
Dental implants have been used to replace teeth for over 50 years, and during that period have enjoyed the highest success rate ever recorded for any medical device inserted into human bone.
The purpose of this article is to inform the community of the Central Valley about what is necessary for proper surgical placement of an orthopedic dental implant into the bones of the skull. An informed public will be better able to make dependable health decisions and thereby avoid injury and jaw deformity.
Understanding Tooth Removal and Bone Repair
Dental implants were designed to fit into the bone region that formerly housed the tooth that was lost, damaged or removed. An understanding of tooth anatomy and the biologic process of bone repair is vital to grasp the scientific principles of dental implant therapy. A natural tooth is anchored to the jawbone via ligament fibers that connect the root portion of the tooth with the wall of the bony socket. Removal of a tooth from the jawbone always results in remodeling of the bony socket leading to bone collapse at the removal site. It has been observed that most of the crestal bone loss occurs on the outside of the jawbone that faces the cheeks or lips. A lesser amount of bone loss occurs on the palate or tongue side of the jawbone (see Figure 1).
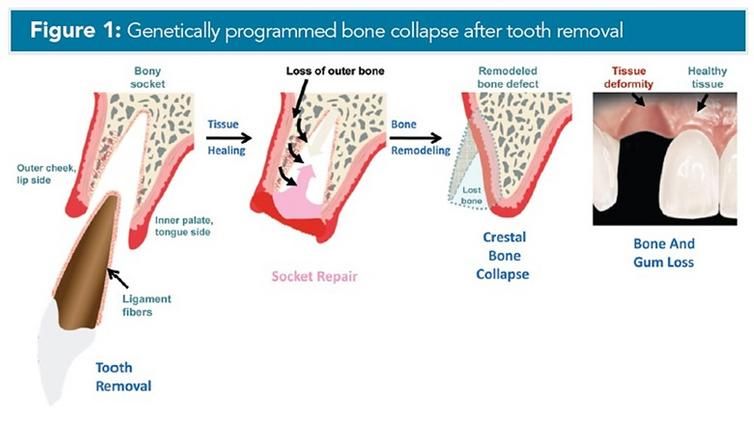
Recent bone healing research has determined that after tooth removal, a bony ridge deformity occurs from the remodeling process resulting in crestal bone collapse. The outer edge of the bone wall is occupied by a genetically-derived bone type called “bundle bone.” The tooth is anchored to the bundle bone and is invested with ligament fibers that provide a vital blood supply to this delicate bone wall (see Figure 2).
Tooth removal results in the loss of tooth ligaments that provide essential bone nourishment. With the removal of the tooth and ligaments, the blood supply to the bundle bone is severed and the bone begins to dissolve away. The bone crest rapidly collapses and is reabsorbed leaving a bony deformity. Because bundle bone is found primarily in the thinner more delicate outer bony region, bone tissue loss will become most pronounced in the highly visible cheek and lip side of the tooth socket. Bundle bone is a tooth-dependent tissue and will always rapidly disappear after tooth removal.
Always Increase the Bone Volume
The only way to prevent bone loss at the time of tooth removal is to graft the bony socket with natural bone in combination with a grafting material that will help to preserve and thicken the local bone volume. If bone grafting is not performed, there will not be a sufficient bone volume available to successfully support a dental implant or provide a great result. Clinical research has demonstrated that a significantly greater amount of bone volume (2-4 mm) is required to maintain a dental implant than is required to house a natural tooth. This large amount of bone thickness required for anchorage of a dental implant does not normally exist and has to be created. Consequently, bone supplementation is a necessity if an implant is to be considered. Since the bundle bone is rapidly lost due to a programmed ridge collapse, bone grafting should ideally be performed at the time of tooth removal. A tooth removed without the benefit of immediate bone grafting may still be repaired at a later time but will likely be more extensive and costly. After bone grafting has been performed, a period of at least 6 months is required for the bone to grow and harden prior to placing a dental implant (see Figure 3).
Surgical specialists with advanced orthopedic training in dental implants are proficient at growing bone and utilize the most advanced materials and latest techniques to create bone volume for dental implant support. Expertise in all the following steps is required for successful bone growth:
- harvesting of natural bone chips
- use of platelet-derived growth factors
- selection of appropriate graft material and collagen membrane
- graft preparation and membrane placement
- specialized orthopedic surgical experience
- a thorough scientific knowledge of bone biology.
Avoid Immediate Implant Placement
In an effort to circumvent bone grafting, many general dentists have attempted to insert a dental implant into the bone socket at the time of tooth removal. This process is called immediate implant placement, “same day implants” or “implants in a day.” Initially, it was believed that dental implant placement at the time of tooth removal would prevent bone socket collapse. However, recent clinical research has conclusively proven that placing a dental implant into a fresh socket cannot prevent collapse of the bony ridge. The bone does not “see” the dental implant and therefore bone remodeling is not influenced by the dental implant device. Bundle bone was lost following dental implant installation due to the genetically programmed collapse. A dental implant is unable to substitute for a tooth immediately following removal and cannot meet the biologic demands or provide the essential blood supply required to retain the delicate bundle bone. It is now well established that dental implant placement immediately into fresh tooth sockets results in loss of the outer bone covering the dental implant and the metal on the dental implant surface becomes exposed. This bundle bone collapse results in gum recession, esthetic concerns and ultimately dental implant failure (see Figure 4).
Immediate dental implant placement has been primarily abandoned by the leading specialists in the field of implant dentistry. Some sites can receive an immediate implant if the wound bed is buried at time of dental implant placement. Immediate dental implant treatment requires exceptional skills, advanced knowledge of bone biology and careful case selection. These skillsets and knowledge are learned in ADA-recognized surgical specialty dental implant training residency.
Several studies have reported unsightly results due to bundle bone collapse and gum recession as soon as 6 months after dental implant placement (see Table 2). This immediate approach to dental implant placement is no longer considered a first line standard of care because of the high incidence of unsatisfactory results and complications that lead to jaw deformity including additional tooth loss. If a tooth is to be extracted, it is critical that bone grafting be performed to prepare the site by increasing the bone volume prior to replacement with a dental implant (see Figure 5).
Efforts to skip the bone building process by immediate insertion of the dental implant will always lead to bone collapse, esthetic nightmares, chronic tissue infection, and eventually implant failure. For successful implantation, it is important to take the time required to complete the necessary steps to achieve a dental implant result that lasts.
Standard of Care for Dental Implant Planning and Placement
It is clear that bone sets the stage for successful dental implants. Therefore, it is essential that bone architecture, volume and density, in addition to the location of nerves and sinus cavities, be assessed prior to dental implant surgery. Since the jawbone is covered by gum tissue, it is impossible to accurately examine the bone structure without the application of CT-scan technology. In the last two decades, breakthrough scientific advances in x-ray imaging have led to the development of Cone Beam CT equipment (CBCT) and software that precisely reveal this vital information in three-dimensions (3D) using a very low radiation dosage. The accuracy of this technology is astounding and affords the clinician the opportunity to do extensive diagnosis, planning and preparation prior to tooth removal, bone grafting and dental implant surgery.
Today, proper diagnosis and planning includes 3D-CBCT-imaging of all proposed implant sites.
3D CBCT-imaging is an essential standard of care for anyone considering dental implant therapy and allows the dental implant team to define parameters of care, treatment limitations and costs pre-operatively. Just as an orthopedic surgeon would not perform a hip or knee replacement without extensive CT imaging and calculations, dental professionals should not proceed with placement of an orthopedic dental implant without CBCT-imaging and precise positional calculations. Traditionally, dentists have mistakenly used standard dental x-rays and mouth molds to determine bone volume and dental implant position. Today, proper diagnosis and planning includes 3D CBCT-imaging of all proposed dental implant sites (see Figure 6).
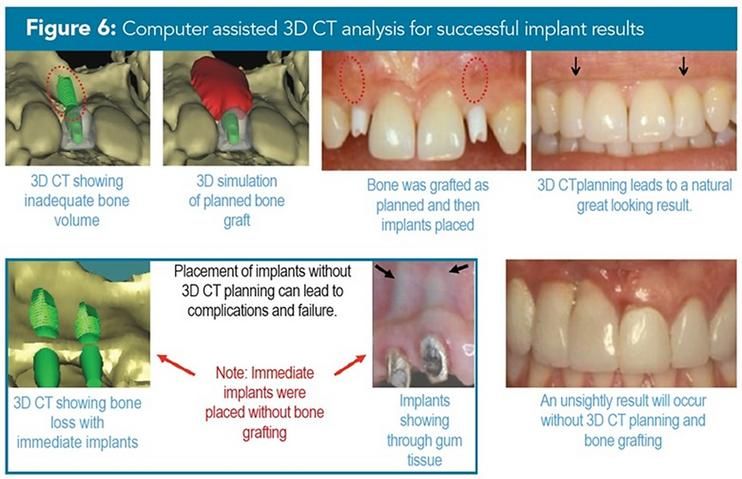
This approach permits 3D site planning for engineering bone and gum tissues and determines all possibilities for proper dental implant positioning and alignment. 3D CBCT analysis and planning changes the surgical approach from speculation to an accurate simulation of the surgery to come. This precise survey permits the surgeon to plan and virtually perform the dental implant surgery in advance, defining in 3D the esthetic and functional demands and costs for dental implants. Once a thorough 3D CBCT examination has been performed, needed bone may be engineered to support a dental implant. Creation of new bone requires approximately 6 months for maturation at which time placement of a dental implant may be considered. Using 3D CBCT data revealing the newly grown bone, precise implant angulation can be determined.
Once the surgeon has defined the ideal dental implant position, customized positioning guides may be constructed from the configured CBCT-data for use during dental implant surgery. The 3D CBCT rendered surgical guide fits upon the adjacent teeth for stability, and precisely guides the dental implant surgeon to deliver the dental implant with proper depth, alignment angle, and positional relationship to the nearby teeth. 3D CBCT-rendered surgical guides permit accurate delivery of this orthopedic medical device into the ideal position for function and beauty. Using surgical guides eliminates misalignment errors and mal-positioning of dental implants thereby reducing complications, undesirable results and dental implant failure. Dental implant placement too close to a nearby tooth will result in loss of bone on that tooth and lead to an unsightly result and eventual tooth loss. For a dental implant to be successful, the standard of care requires precise dental implant placement using such computer-guided technology.
Framing The Tooth
Once a dental implant is properly placed, a period of 2-3 months is required for union of this orthopedic device with the bone. The next step is to develop the gum tissue around the implant so that it will adapt to the final porcelain crown which simulates a natural tooth (see Figure 7).

No one individual can master all the steps and all the complexities of the implant process. Find out for yourself who is most qualified to provide the excellence you deserve when considering implants.
The purpose of gum tissue is to cover and protect the jaw bone from the mouth and to form a seal around teeth. If a smaller volume of bone is present, then there will also be a smaller amount of gum tissue framing a tooth. Similarly, gum tissues also form a seal around dental implants protecting the bone which is in union with the implant. Because gum tissues around a dental implant have a reduced blood supply and supporting fiber network when compared to a native tooth, it is very difficult to make a dental implant tooth look like a real tooth. In order to create sufficient amount of gum tissue to frame a dental implant, it is necessary to engineer an appropriate bony tissue base as described earlier. Newly created bone with orthopedic grafting provides a nourishing framework that supports the gum tissues that encase a dental implant crown. The gum tissue bed that frames the crown is shaped and contoured using customized acrylic temporaries over a period of several months. Exquisite temporary crowns must be modified every few weeks to develop a natural gum geometry surrounding the dental implant.
Choose A Dental Implant Surgical Specialist
Finding the right team is essential to a successful dental implant experience (see Table 3).
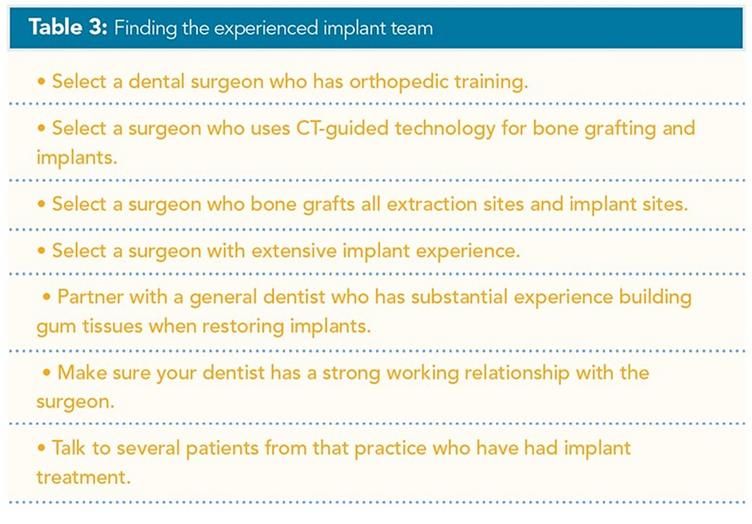
Since bundle bone always collapses after tooth removal and bone grafting is essential for dental implant support, it is critical that you find an experienced team that includes a dental implant surgical specialist with orthopedic training (Periodontics and Oral Surgery). Another vital member of the team is a knowledgeable general restorative dentist with proven experience in building gum contours when restoring dental implant crowns. No one individual can master all the steps and all the complexities of the dental implant process. Find out for yourself who is most qualified to provide the excellence you deserve when considering dental implants. Do your own research, seek multiple opinions and ask the specific questions that help you discern the best dental implant specialist for your dental implant needs.
Questions that you should ask when selecting your dental implant specialist include:
- What type of orthopedic specialty training in dental implants and bone grafting have you received?
- How long have you been placing dental implants?
- How many dental implants have you placed over your career?
- Do you place dental implants immediately into extraction sites?
- What is the scope of bone graft training you have received?
- Do you believe bone grafting is necessary?
- How will you know if I have enough bone for a dental implant?
- Do you require a CBCT-scan to do your dental implant diagnostic planning?
- Do you use CBCT-rendered surgical guides for dental implant positioning?
- How do you develop the gum tissue around the dental implant?
- How well do you work with my restorative dentist?